When you feel/see stroke-like symptoms, Time is Brain!When you present to the Emergency Department with stroke-like symptoms, there are a variety of tests that can be done: |
|
 |
CT Scan (of head without contrast)
A CT scan uses X-rays to produce a 3-dimensional image of your head. A CT scan can be used to diagnose ischemic stroke, hemorrhagic stroke, and other problems of the brain and brain stem. CTA Scan (Head/Neck) Medical test that combines a CT scan with an injection of a special dye to produce pictures of blood vessels and tissues in a part of your body. The dye is injected through an intravenous (IV) line started in your arm or hand. A computerized tomography scan, or CT scan, is a type of X-ray that uses a computer to make cross-sectional images of your body
|
| Evaluations by various providers Some of these providers can include:Stroke Neurologist and ER Physician– these professionals determine the next steps and decide which treatment option is best. Discussion about possible treatments if patient is eligible/appropriate for treatment such as thrombolysis and/or thrombectomy.Pharmacy Team – this team is responsible for determining which medications are best for each patient, taking into consideration the medications this patient takes at home and medical history related to anticoagulants. |
 |
 |
Neurological Assessment
This test is used to quantify neurologic impairment is the National Institutes of Health Stroke Scale (NIHSS). The NIHSS enables the healthcare provider to rapidly determine the severity and possible location of the stroke. |
|
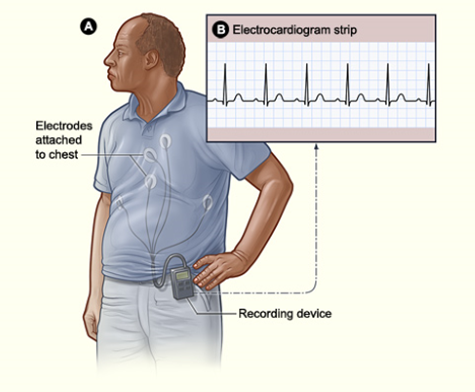
EKG Electrocardiogram (EKG) is a test to help detect heart problems. This is a standard test performed to help determine if heart problems caused the stroke. |
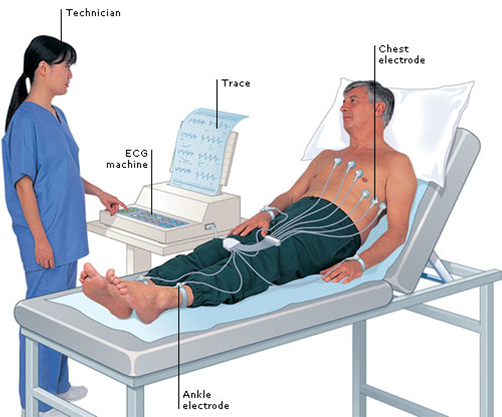 |
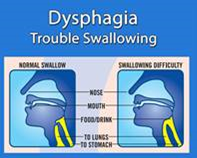 |
Bedside Swallowing Evaluation
This evaluation helps measure the patient’s swallowing abilities. This test assesses the risks for choking and also helps with dietary recommendations. The provider will closely monitor you and test your ability to swallow different substances. One the assessment shows you are at low risk, you will be cleared to eat. Until this happens, you may hear that your provider has instructed your nurses and caregivers that you are NPO (nothing by mouth). |
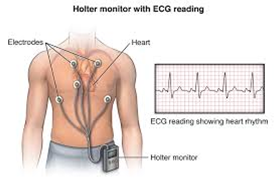
| Monitoring of Heart Rhythm and Telemetry
Atrial Fibrillation (A-fib) is the most frequent cause of ischemic stroke in the elder population. Telemetry can capture these cardiac problems in stroke patients and can help providers get a better overall picture of how to best care for their patient. |
 |
Upon completion of the above tests, you could be admitted to the hospital.Once admitted to the hospital, there are many other tests that can be done: |
|
| MRI (Magnetic resonance imaging, MR)
An MRI uses magnetic fields to produce a 3-dimensional image of your head. The MR scan shows the brain and spinal cord in more detail than CT. MR can be used to diagnose ischemic stroke, hemorrhagic stroke, and other problems involving the brain, brain stem, and spinal cord. |
 |
 |
Echocardiogram (2-d echo, Cardiac echo, TTE, TEE)
Painless ultrasound waves are used to take a picture of your heart and the circulating blood. The ultrasound probe may be placed on your chest (trans-thoracic echocardiogram, TTE) or deep in your throat (trans-esophageal echocardiogram, TEE). |
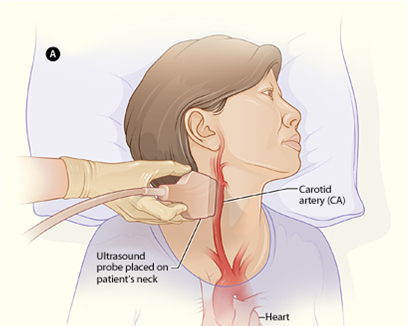
| Doppler Studies of Neck
This is a non-invasive test that uses sound waves to detect narrowing of your arteries or potential blockages caused by plaque. It helps your healthcare provider determine if you are at risk of having a stroke and if there is a need to prescribe preventative measures. |
 |
 |
Angiogram
This procedure involves the injection of a colorful dye into the carotid artery through a catheter. Radiographs are taken as the dye flows through the brain. This test can be used to identify different problems in the brain such as: bleeding aneurysms, vasospasm, and arteriovenous malformations, and to differentiate embolism from large artery thrombosis. |
| Bloodwork
There is no blood test that can indicate stroke, but the doctor or nurse may do a series of blood tests to learn the cause of your stroke. These tests provide information about the stroke risk factors and other medical problems that will aid in determining the best way to prevent another stroke. |
 |
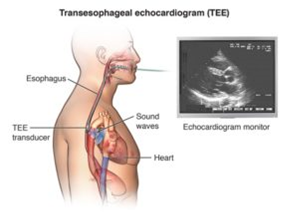 |
Trans-Esophageal Echocardiogram
This test provides images of the internal structures of the heart and its blood vessels using the same ultrasound technology as an echocardiogram. This test is useful in detecting any sources of blockage within the midsection of the body (thoracic region). Any blockage like this may lead to lack of oxygen in the brain and may cause a stroke. |
| External Cardiac Monitor and/or Implantable Loop recorder at discharge
This is a device that monitors heart rhythm and activity. Sometimes a patient may be asked to use one of these to monitor for atrial fibrillation or other abnormal heart activity. This device can help detect causes of fainting, palpitations, very fast or slow heartbeats, and hidden rhythms that can cause strokes. This device is both external and implantable. Typically, this is a device that is used after a patient has an ischemic stroke and further helps find the root cause of the stroke. |
 |
Supporting Services in Stroke CareStroke patients can expect to see a couple of these specialists during their stay at the hospital. Each discipline plays an important role in stroke care and recovery. |
|
 |
Physical Therapy
Therapists who are trained in all aspects of anatomy and physiology related to normal function, with an emphasis on movement. They help stroke survivors to regain strength, coordination, balance, and control of movement including walking, climbing stairs, getting into and out of bed. |
 |
Speech Therapy
Therapists who assess and treat communication and swallowing disorders after stroke. Stroke therapists help stroke patients who suffer from Aphasia. This is a common symptom characterized as the inability to express oneself or understand others. The most common way to regain this ability is through speech therapy. |
 |
Occupational Therapy
Therapists who provide a holistic approach (mind, body, spirit, and emotion) to help people reach the greatest level of function (activities of daily living) and independence to achieve the best result for health improvement during stroke recovery. |
 |
Cardiology
Doctors who specialize in taking care of the heart. They determine if you have any heart problems that may have caused your stroke. |
 |
Pharmacist
These professionals advise other healthcare professionals about safe and effective medicines to use. Pharmacists also ensures that the pharmacy and systems are fit for practice. Pharmacists are responsible for helping you understand the medications given to you during and after stroke. |
 |
Diabetes Team
Diabetes is a large factor when calculating stroke risk. With diabetes, your chances of having a stroke are much higher. Typically this team has an endocrinologist who can help teach the patient how to manage their diabetes and reduce their risk of stroke. |
 |
Case Management/ Social Service Team
Stroke patients and families of the patients may be overwhelmed and need support and compassion. These professionals can assist in finding support groups, therapy, and any other assistance the patient needs. Social services team is not just here for the patient, but can help support friends and family affected as well. |
 |
Neurosurgery
These specialists play a vital role in stroke care. Neurosurgery fulfils essential requirements for treating stroke patients. Neurosurgeons provide the patients with procedures such as Mechanical Endovascular Retrieval (MER) where a catheter is used to navigate and retrieve blood clots and restore good blood flow within vessels. |
 |
Neurocognitive Evaluation Team
This team performs and analysis is tests of the brain that measure brain function in a non-invasive way. The tests done are specifically crafted to measure particular parts and functions of the brain. By measuring these different aspects, the neurocognitive evaluation team can get a good picture of what is happening with the patient’s brain. |